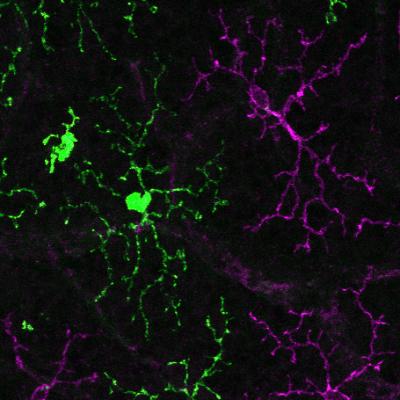
Transplanted human lab-grown microglia (green) and native mouse microglia (magenta) team up to rebuilt a local immune network in the mouse retina. Credit: Wenxin Ma, Robert Fariss, Wai Wong, and Wei Li
NEI researchers have successfully transplanted human microglia cells into mouse retina to create a model that could be used to test new treatments for incurable eye diseases.
Microglia are the innate immune cells of the central nervous system, which includes the retina, and play essential roles in the normal development of nerves and nerve connections (synapses). But they can also switch to a more sinister role – driving the development of brain and eye diseases, including age-related macular degeneration (AMD), glaucoma, diabetic retinopdathy and uveitis (inflammation of the eye). Under normal conditions, microglia vigilantly survey environmental changes to maintain normal retinal function. Under pathological conditions, they will respond quickly to injuries, but could also become inappropriately activated, grow in number, and migrate into surrounding tissues.
“Our understanding of microglia function comes predominantly from rodent studies due to the difficulty of sourcing human tissue and isolating the microglia from these tissues. But there are genetic and functional differences between microglia in mice and humans, so these studies may not accurately represent many human conditions,” said lead author Wenxin Ma, Ph.D., biologist, NEI Retinal Neurophysiology Section.
The research, published today as a Reviewed Preprint in eLife, is described by the editors as an important study with solid data demonstrating the potential for microglial replacement therapy to treat retinal and central nervous system diseases.