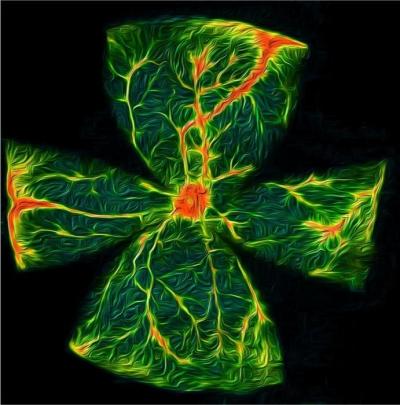
Artistic rendition of a diabetic mouse retina demonstrating retinal vasculature (yellow) with increased leakage (red) following insulin-induced transient episode of hypoglycemia (low glucose). Credit: Isabella Sodhi, McDonogh School
In a new National Institutes of Health-funded study led by scientists at the Wilmer Eye Institute, Johns Hopkins Medicine researchers say they have determined that low blood sugar, or hypoglycemia, may promote a breakdown of the blood-retinal barrier, an important boundary that regulates the flow of nutrients, waste and water in and out of the retina.
The research, which investigated the phenomenon in diabetic mice, provides insights into the origin of diabetic retinopathy, specifically in patients with episodes of hypoglycemia. Diabetic retinopathy, a severe complication of both type 1 and type 2 diabetes, can cause permanent vision damage if left untreated.
The full study, published in Science Translational Medicine on April 30, explains that a specific protein known as hypoxia-inducible factor (HIF) accumulates in certain cells in the retina during periods of low blood sugar.
HIF has been implicated in diabetic retinopathy and other eye diseases before. The protein can trigger a chain reaction, switching on overproduction of other proteins which lead to overgrowth and leakage of blood vessels in the retina. Now, scientists have found that HIF is a player in how the blood-retinal barrier breaks down during hypoglycemia.
Researchers tested HIF’s role in hypoglycemia by inducing periods of low blood sugar in mice with and without diabetes. Their experiments showed that mice with diabetes had higher levels of HIF during hypoglycemia, enough to promote the breakdown of the blood-retinal barrier and cause leakage in retinal blood vessels, while mice without diabetes did not experience higher levels of HIF. This breakdown in diabetic retinopathy contributes to irreversible damage to the retina and vision loss.
The team investigated further by testing an experimental drug known as 32-134D, which inhibits the HIF protein. Some diabetic mice received an injection of 32-134D prior to induced episodes of low blood sugar, and researchers observed lower HIF levels, in turn preventing the expression of proteins that promote the breakdown of the blood-retinal barrier and blood vessel leakage.
“These studies help explain why patients with diabetes who are initially started on tight glucose control, the cornerstone of diabetic management, or those who have high glycemic variability (transient episodes of very low — followed by very high — serum glucose levels), experience worsening of their diabetic eye disease,” says corresponding author Akrit Sodhi, M.D., Ph.D., associate professor of ophthalmology and the Branna and Irving Sisenwein Professor of Ophthalmology at the Johns Hopkins University School of Medicine and the Wilmer Eye Institute. “Our findings underscore why therapies targeting HIF will be an effective approach to prevent or treat diabetic retinopathy.”
To read more, go to Johns Hopkins News