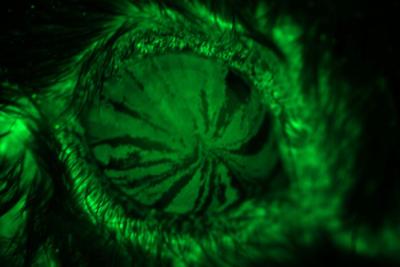
By tracking the movements of stem cells (in fluorescent green) in a mouse eye, researchers were able to trace the cells as they differentiated into corneal cells and migrated to the center of the cornea, providing clues about how the cells work to help corneal injuries heal. Image credit: Washington University in St. Louis
People with a condition known as dry eye disease are more likely than those with healthy eyes to suffer injuries to their corneas. Studying mice, researchers at Washington University School of Medicine in St. Louis have found that proteins made by stem cells that regenerate the cornea may be new targets for treating and preventing such injuries.
The researchers analyzed genes expressed by the cornea in several mouse models — not only of dry eye disease, but also of diabetes and other conditions. They found that in mice with dry eye disease, the cornea activated expression of the gene SPARC. They also found that higher levels of SPARC protein were associated with better healing.
“We conducted single-cell RNA sequencing to identify genes important to maintaining the health of the cornea, and we believe that a few of them, particularly SPARC, may provide potential therapeutic targets for treating dry eye disease and corneal injury,” said first author Joseph B. Lin, an MD/PhD student at Washington University School of Medicine in St. Louis.